The past, present and future of antiviral discovery
Just over a year ago, the first two SARS-CoV-2 vaccines were released in record time. While they have been crucial for mitigating the spread of the virus, there is currently only one treatment approved by the U.S. FDA for the disease. The lack of effective antiviral drugs is not unique to COVID, however. From rhinovirus to influenza, herpes simplex virus and HIV, treating viral infections has been a constant battle, with few drugs able to claim victory. Fortunately, even before COVID-19 took over our lives and laboratories, the pharmaceutical industry was hard at work developing methods and strategies to address the complexities of viral infection and antiviral drug development.
The growing threat of viruses
The COVID-19 pandemic is the largest viral outbreak in a century and yet some epidemiologists believe that it is only a sign of things to come. An increase in global travel, urbanization and deforestation, as well as changing agricultural practices and climate change, create a perfect storm for elevated infection risk. These types of large-scale changes increase our exposure to animals that carry deadly viruses and facilitate faster animal-to-animal and human-to-human spread. Outbreaks that begin from animal-to-human transmission have also increased over the last several decades, and there is no indication that this trend will abate.
Following the successful development of mRNA-based vaccines against COVID-19, more efficient vaccine development is on the horizon. But due to various manufacturing challenges, as well as wavering vaccine supply, access, demand and effectiveness, vaccines alone are not enough to quell an outbreak. The world needs effective therapeutics, too. However, scientists have struggled to find effective antivirals against many viruses, even those that have plagued humanity for centuries.
Why viruses are so difficult to treat
Antibiotics work by targeting molecules or enzymatic reactions taking place in bacterial cells, which feature many druggable targets including proteins that mediate metabolism and reproduction. Viruses, on the other hand, hide inside host cells and do not contain much material to target. They also do not perform crucial processes on their own; a virus’ only function is to replicate, and it uses its host cell’s machinery to do it. Because the virus relies on the biological machinery of cells, it is challenging to develop a drug that selectively targets the virus but leaves the host cell undamaged.
Furthermore, viruses mutate quickly, making them a moving target. For example, although SARS-CoV-2 first appeared just over two years ago, scientists have already identified thousands of variants. Still, SARS-CoV-2 mutates at only half the rate of influenza and a quarter of the rate of HIV. As seen with the delta and omicron variants of SARS- CoV-2, variants can contribute to a virus’ transmissibility and infection severity and threaten to sidestep the immunity provided by vaccines. Taking all these variables into account, the key to identifying an effective antiviral drug is developing a molecule or delivery method that targets a portion of the virus that does not easily mutate.
How antivirals are made
Viral particles generally exhibit a specific set of behaviors, which antiviral developers seek to disrupt. While scientists have been working to develop effective antivirals for more than half a century, each research team has had at least one of two goals in mind when building their drug candidates: either blocking viruses from entering cells or pre- venting them from replicating.
For example, the first antiviral drug ever approved by the FDA, idoxuridine, does the latter: It replaces a nucleotide in the HSV-1 genome and tangles up its replication machinery, preventing the herpes virus from making copies of itself.
More recently, an antiviral HIV cocktail uses a combination of both methods to mitigate infection: The drug regimen targets the entry of the virus into T-cells and the reverse transcription process to prevent integration into the host genome. HIV is a rare success story in the history of antiviral development where antivirals have transformed HIV from a deadly disease into a chronic illness. Although the pharma industry has made great strides in the treatment of HIV, additional therapeutics are needed for a variety of other viral infections, including COVID-19.
Identifying treatments for COVID-19
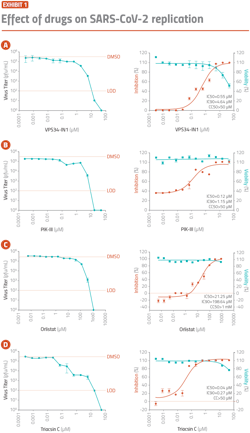
Researchers tested several compounds at various concentrations against a human airway epithelial cell line infected with SARS-COV-2 and monitored inhibition of viral replication over the course of 72 hours using a bioelectronic assay. They found that attenuating VPS34 kinase activity and fatty acid metabolism successfully inhibited SARS-CoV-2 replication. — Williams et al. Cell Rep. 2021; 36(5): 109479.
Despite the development of several vaccines designed to prevent the spread of SARS-CoV-2, COVID-19 is expected to become endemic like the flu. Since eradicating the virus is unlikely, the development of therapeutics that reduce the severity of infection is essential.
The first FDA-approved treatment for SARS-CoV-2 infection was remdesivir. This drug borrows idoxuridine’s strategy of sneaking into the viral genome and stalling replication. Remdesivir, however, has been subject to controversy surrounding its purported efficacy against COVID-19 and other infections. Scientists are therefore continuing to develop novel antivirals specific to the virus.
Given SARS-CoV-2’s tendency to mutate on a regular basis — by some reports, at least twice every month — scientists in pursuit of an antiviral against SARS-CoV-2 are following the path that researchers took with HIV. They are looking to target not the viral genome, but the mechanisms by which it enters cells and replicates. In fact, Pfizer’s recently authorized oral COVID-19 medication consists of a combination of protease inhibitors, including one that is used to treat HIV. This drug, like others in development, blocks SARS- CoV-2 replication.
Coronaviruses replicate in a unique way, which makes the process an especially promising target for antiviral therapy. Coronaviruses make copies of themselves in replication organelles. Previously, scientists found that targeting these organelles was an effective way of reducing the severity of infection from several different types of viruses. For example, inhibiting VPS34, a protein central to cell membrane biology, hampers the replication of hepatitis C virus, tombusvirus, and other coronaviruses. Recently, Christopher Basler, Ph.D., and his team at Georgia State University used a bioelectronic assay to continuously monitor cell health for 72 hours and discovered that inhibiting VPS34 reduces the degree to which SARS-CoV-2 infection leads to cell death in vitro in a dose-dependent manner.*
The team employed the same bioelectronic assay to monitor the inhibitory effects of two drugs that support fatty acid metabolism, another pathway needed for the formation of replication organelles. As predicted, the team discovered that both drugs, orlistat and triacsin C, inhibited SARS-CoV-2-induced cell death. This work opens the door to potential therapeutic development.
Let’s not forget about influenza
Among the viruses that worry epidemiologists, SARS-CoV-2 is just the most recent. The influenza virus, in contrast, has threatened public health for centuries. In the last decade, the flu has caused nearly 360,000 deaths and nearly 4.5 million hospitalizations in the U.S. alone. New variants develop regularly, leading to at least one epidemic per generation wherein the affected population has no immunity to the strain. Given the ongoing threat of the influenza virus, the world needs effective antivirals against it.
The FDA has approved at least six drugs to treat the flu, but the CDC only recommends using four of them because several show limited clinical benefit. The first drug approved to treat the flu, amantadine, and its derivative rimantadine, are no longer used because of the emergence of resistant strains. Today, commonly used neuraminidase inhibitors are heading in the same direction. As evidenced by the epidemiological data, the drugs available today are not sufficient for minimizing hospitalizations and deaths.
The future of antiviral development against influenza will require targeting regions of the virus that do not mutate often. Incidentally, several antibody treatments in clinical trials today are examining a conserved portion of the same protein that the immune system naturally targets: the hemagglutinin protein. Hemagglutinin projects out from the viral membrane and helps the influenza virus enter cells. Scientists are hoping to develop antivirals against its ‘stem’ to disrupt the protein’s function.
This novel approach is part of a larger trend to develop antibodies that can serve as broad-spectrum antivirals effective against more than one virus family.
The current status of broad-spectrum antivirals
To identify effective broad-spectrum antivirals, researchers expose cells to candidate antivirals at different concentrations and test if the drug reduces cell death caused by infection. The drugs are typically tested on cell lines, though primary cells or stem cell-derived cultures may also be used.
Such in vitro studies have indicated the potential benefit of some broad-spectrum antivirals against influenza and COVID-19. For instance, favipiravir, an oral form of remdesivir that disrupts viral replication, has shown efficacy against 53 strains of the influenza virus and moderately positive effects against Ebola and several other lethal viruses. Currently, researchers around the world are studying the drug’s potential benefit in people with COVID-19. Another promising broad-spectrum antiviral candidate is IFN-, a naturally occurring cytokine that contributes to the body’s antiviral response. As a drug, it has shown efficacy in cell and animal models against influenza A and several other viruses.
Unfortunately, despite dozens of studies in cells and animals, most nucleic acid- and protein-based antivirals so far have shown limited efficacy against their intended targets. To aid in the development of broad-spectrum antivirals, engineers have begun investigating the potential benefits of an entirely different class of therapeutics: novel materials.
Materials scientists join the search
Several synthetic materials under development today show promise as broad-spectrum antivirals. For example, scientists developed an antiviral nanoparticle that is coated with a molecule that mimics a cell surface receptor used by viruses to bind to cells. This nanoparticle successfully inhibits infection from several viruses, including HSV, human papillomavirus, dengue virus and others. Researchers have also synthesized materials to mimic the phospholipids that compose the cell membrane. These molecules successfully block enveloped viruses, including hepatitis C and HSV-1 and -2, from fusing with cells. Influenza viruses and coronaviruses are also enveloped, suggesting a broader application for these materials.
While the concept of using synthetic materials as antiviral drugs is still in its infancy, data suggests that they could offer an alternative approach to antiviral development.
More work to do
The COVID-19 pandemic made the dearth of therapeutic options available to people suffering from viral infections obvious. Despite numerous attempts to develop antivirals over the past several decades, most candidates have shown limited clinical success.
But there is hope. Scientists are finding success targeting the coronavirus replication cycle, suggesting more treatments for COVID-19 are within reach. Furthermore, the field of broad-spectrum antiviral research is burgeoning. Researchers are discovering potential treatments against previously untreatable viruses. Like currently available HIV treatments, future successful antivirals will likely involve combinations of drugs that target numerous aspects of viral entry and replication in host cells. Combined with a broad-spectrum approach using synthetic materials, these treatments could generate a new path towards treating deadly viruses, from SARS-CoV-2 to influenza and beyond.